Category: Blood Health & Chronic Conditions
Estimated Reading Time: 7 minutes
Published by: Yarima.org Health Team
🩸 What Is Sickle Cell Disease?
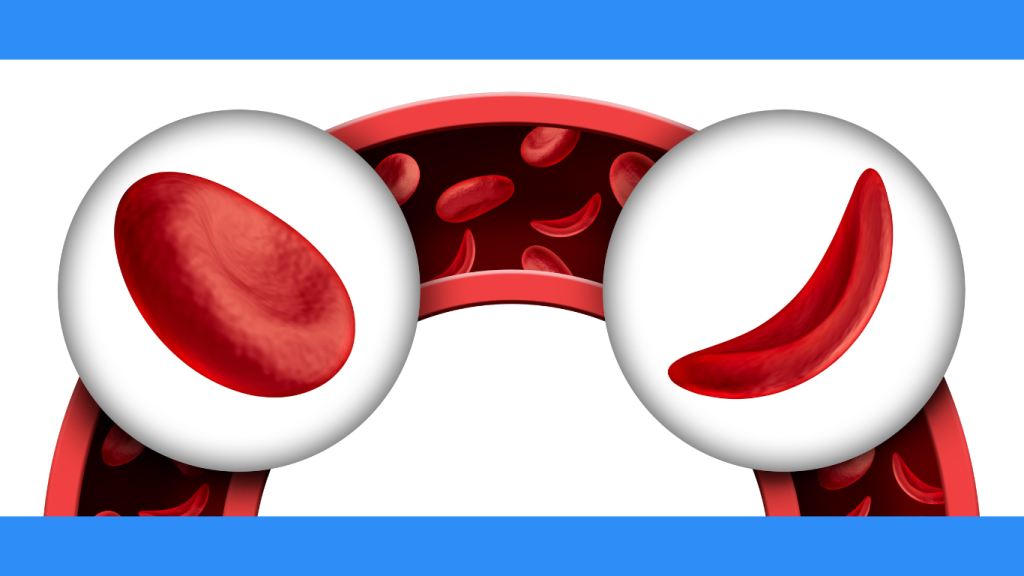
Sickle Cell Disease (SCD) is a group of inherited blood disorders that affect hemoglobin — the protein inside red blood cells that carries oxygen throughout the body.
In SCD, red blood cells become C-shaped (sickled), stiff, and sticky instead of round and flexible.
These sickled cells:
- Break apart easily
- Block blood flow
- Cause painful episodes
- Reduce oxygen delivery to organs
This combination can lead to serious health complications if not properly managed.
| Type | Genotype | Severity |
|---|---|---|
| SS | S + S | 🔥 Most severe |
| SC | S + C | Moderate |
| Sβ⁰ | S + β⁰ | Severe |
| Sβ⁺ | S + β⁺ | Mild–moderate |
| AS (trait) | A + S | Not a disease but carrier |
🧬 What Causes Sickle Cell Disease?
SCD is caused by a genetic mutation in the HBB gene, which affects hemoglobin production.
To have SCD, a person must inherit:
- One sickle cell gene from each parent
If only one gene is inherited, the person has sickle cell trait, not the disease. They usually do not have symptoms but can pass the gene to their children.
SCD is more common among people with ancestors from:
- Africa
- The Caribbean
- Middle East
- South America
- Central America
- India
- Mediterranean regions
💥 Symptoms of Sickle Cell Disease
Symptoms vary, but common issues include:
1. Pain Crises (Vaso-Occlusive Episodes)
Sudden, intense pain caused by blocked blood flow. Pain may occur in:
- Chest
- Arms
- Legs
- Back
- Abdomen
2. Anemia
Sickled cells break down faster than the body can replace them → chronic fatigue, weakness, shortness of breath.
3. Frequent Infections
Damage to the spleen makes the body less able to fight bacteria.
4. Swelling of Hands and Feet
Due to blocked blood circulation.
5. Delayed Growth in Children
Lack of oxygen and nutrients slows development.
6. Jaundice
Yellowing of skin and eyes because of rapid red blood cell breakdown.
🚨 Possible Long-Term Complications
If unmanaged, SCD can contribute to:
- Stroke
- Acute chest syndrome
- Organ damage (kidney, liver, lungs)
- Vision problems
- Leg ulcers
- Gallstones
- Priapism in males
Early care and consistent monitoring greatly reduce these risks.
🛡️ How to Manage Sickle Cell Disease
Although there is no universal cure, SCD can be managed effectively with medical care, lifestyle habits, and prevention strategies.
✔️ 1. Medical Treatments
Hydroxyurea
Helps reduce pain crises and the need for blood transfusions.
Blood Transfusions
Increase normal red blood cells to improve oxygen levels and reduce stroke risk.
Bone Marrow/Stem Cell Transplant
The only known cure — but requires a matched donor and is not suitable for everyone.
Antibiotics & Vaccines
Children are often given daily penicillin and must stay up to date on vaccines to prevent infections.
Pain Management
May include anti-inflammatory medicines or doctor-prescribed treatments during severe crises.
✔️ 2. Daily Habits to Reduce Crises
Healthy habits can help maintain blood flow and prevent crisis triggers:
- Stay hydrated
Dehydration increases sickling. - Avoid extreme temperatures
Both heat and cold can trigger pain episodes. - Manage stress
Stress hormones can worsen symptoms. - Get enough sleep
Supports overall health and immunity. - Avoid high altitudes and low-oxygen environments
Airplane cabins, mountains, or poorly ventilated places may trigger crises.
✔️ 3. Nutrition for Support
A nutrient-rich diet helps support energy and immunity:
- Leafy greens (folate & iron support red blood cell formation)
- Lean proteins
- Colorful fruits and vegetables (antioxidants help reduce inflammation)
- Omega-3 foods (fish, walnuts) for circulation and inflammation control
✔️ 4. Infection Prevention
Because infections are dangerous for people with SCD:
- Stay up to date with vaccines (flu, pneumonia, meningitis)
- Wash hands frequently
- Treat fevers immediately — fevers can be emergencies
- Seek medical help if experiencing chills, chest pain, or breathing difficulty
❤️ Living Well With Sickle Cell Disease
With proper care, many people with SCD:
- Attend school
- Work full-time
- Have families
- Live long, healthy, fulfilling lives
Early diagnosis, consistent medical care, healthy habits, and strong support systems make a powerful difference.
🔍 Bottom Line
Sickle Cell Disease is a genetic condition that affects how red blood cells carry oxygen.
While it can cause pain and complications, understanding the disease — and actively managing it — greatly improves quality of life.
Hydration, good nutrition, medical care, infection prevention, and stress control are key pillars of staying healthy with SCD.
📚 References
- National Institutes of Health (NIH) – Sickle Cell Disease
https://www.nhlbi.nih.gov/health/sickle-cell-disease - Centers for Disease Control and Prevention (CDC) – Sickle Cell Disease
https://www.cdc.gov/ncbddd/sicklecell/index.html - National Library of Medicine (NIH) – SCD Overview
https://www.ncbi.nlm.nih.gov/books/NBK1377/