Category: Gut Health & Chronic Disease
Reading Time: ~6 minutes
Published: January 7, 2025
Published by: Yarima.org Team
Ulcerative colitis is a chronic inflammatory condition of the digestive system that affects millions of people worldwide. While it is often grouped under inflammatory bowel disease (IBD), ulcerative colitis has unique features, triggers, and management strategies that are important to understand.
This condition can feel overwhelming—but with the right knowledge and lifestyle support, many people are able to reduce flare-ups and improve quality of life.
Let’s break it down in a simple, science-based way.
What Is Ulcerative Colitis?
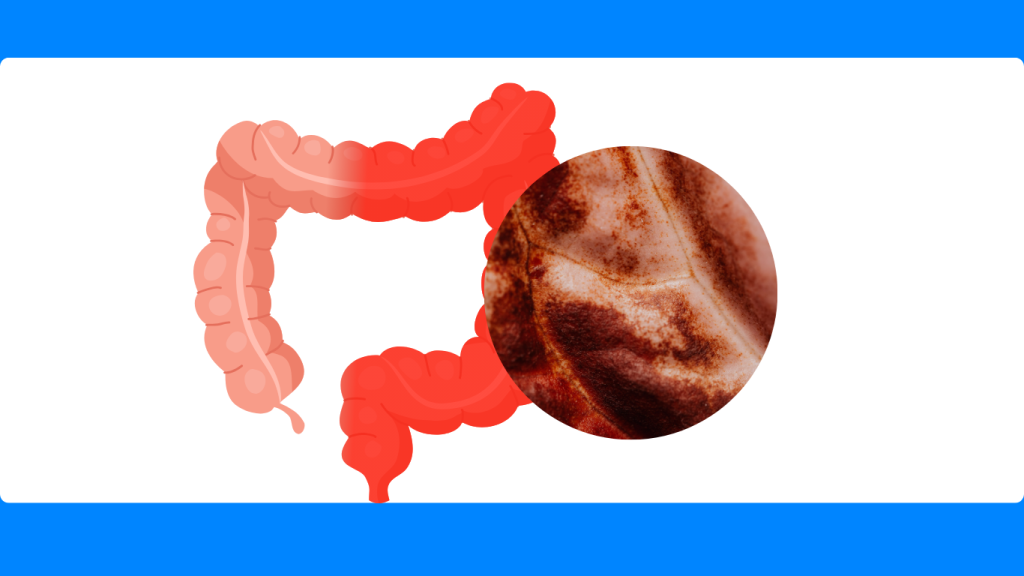
Ulcerative colitis (UC) is a chronic inflammatory disease of the colon (large intestine). It causes inflammation and small ulcers to form along the inner lining of the colon and rectum.
Unlike Crohn’s disease, which can affect any part of the digestive tract, ulcerative colitis:
- Affects only the colon and rectum
- Involves continuous inflammation, not patchy areas
- Primarily impacts the inner lining of the gut
UC usually follows a pattern of flare-ups and remission.
What Causes Ulcerative Colitis?
There is no single cause, but research shows ulcerative colitis develops from a combination of factors.
1. Immune System Dysfunction
In UC, the immune system mistakenly attacks the lining of the colon, triggering chronic inflammation—even when no infection is present.
2. Gut Microbiome Imbalance
An unhealthy balance of gut bacteria can overstimulate the immune system and weaken the intestinal barrier, increasing inflammation.
3. Genetic Susceptibility
People with a family history of inflammatory bowel disease have a higher risk, suggesting genetics play a role.
4. Environmental and Lifestyle Triggers
Certain factors may worsen or trigger symptoms:
- Highly processed foods
- Refined carbohydrates and sugars
- Chronic stress
- Poor sleep
- Smoking history (especially after quitting)
Common Symptoms of Ulcerative Colitis
Symptoms vary depending on disease severity but often include:
- Chronic diarrhea
- Blood or mucus in stool
- Abdominal pain or cramping
- Urgency to use the bathroom
- Fatigue
- Unintended weight loss
- Anemia (from blood loss)
During flare-ups, symptoms can become intense and disruptive.
How Ulcerative Colitis Affects the Body
Ongoing inflammation in the colon can:
- Reduce nutrient absorption
- Increase intestinal permeability (“leaky gut”)
- Lead to dehydration and electrolyte imbalance
- Increase the risk of colon complications if unmanaged
This is why long-term management—not just symptom control—is essential.
Managing Ulcerative Colitis: Diet & Lifestyle Support
While medical treatment is often necessary, diet and lifestyle play a powerful supportive role.
1. Reduce Inflammatory Triggers
Many people benefit from limiting:
- Refined sugars
- Ultra-processed foods
- Industrial seed oils
- Alcohol during flares
These foods can worsen inflammation and irritate the gut lining.
2. Focus on Gut-Friendly Nutrition
During remission or mild symptoms, supportive foods may include:
- Well-cooked vegetables
- Lean proteins
- Omega-3–rich foods (fatty fish)
- Fermented foods (if tolerated)
- Soluble fiber (introduced slowly)
During flares, softer, low-residue foods may be better tolerated.
3. Support the Gut Barrier
Nutrients that support intestinal lining health include:
- Zinc
- Glutamine
- Vitamin D
- Omega-3 fatty acids
A stronger gut barrier helps calm immune overreaction.
4. Manage Stress
Stress does not cause UC, but it can worsen symptoms by activating inflammatory pathways. Helpful tools include:
- Mindfulness
- Breathing exercises
- Gentle movement
- Adequate rest
5. Prioritize Sleep and Recovery
Poor sleep disrupts immune regulation and increases inflammation. Consistent sleep supports remission and healing.
Can Ulcerative Colitis Be Cured?
Currently, there is no known medication that can cure, but surgery (in severe or unresponsive cases) can be an option. Ulcerative colitis can be effectively managed. Many people achieve long periods of remission with the right combination of medical care, nutrition, and lifestyle support.
Early management and consistent follow-up reduce the risk of complications.
When to Seek Medical Care
Immediate medical attention is needed if symptoms include:
- Severe abdominal pain
- Heavy bleeding
- Fever
- Rapid weight loss
- Signs of dehydration
Regular monitoring is important even during remission.
Key Takeaway
Ulcerative colitis is a chronic condition—but it does not define your future. Understanding how inflammation, immunity, and gut health interact empowers you to make choices that support healing, reduce flare-ups, and protect long-term digestive health.
Knowledge is one of the most powerful tools in managing chronic disease.
📚 References
- National Library of Medicine (PMC): Inflammatory Bowel Disease
- Crohn’s & Colitis Foundation
- Cleveland Clinic: Ulcerative Colitis Overview